Minimally Invasive Aortic Valve Replacement
Minimally-invasive aortic valve repair is cardiac surgery performed to treat stenosis (narrowing) and regurgitation (leakage) of the aortic valve. The aortic valve connects the left ventricle of the heart with the aorta, the body's largest artery, from where oxygenated blood is pumped to the rest of the body
Minimally-invasive aortic valve replacement is an alternative kind of valve replacement that does not require a large incision, known as a median sternotomy. It is instead performed with a smaller incision on the upper breastbone known as a mini-sternotomy. The surgery is performed under general anaesthetic and a heart-lung bypass machine is used.

The damaged or diseased aortic valve is removed and a prosthetic valve inserted, which may be either biological (made of animal tissue) or mechanical. Which valve is used depends on the patient's age, lifestyle, medical conditions and preferences.
A mechanical valve will last indefinitely, but carries a higher risk of blood clotting problems. This means that patients that opt for a mechanical valve will have to take anticoagulant medicine for the rest of their lives.
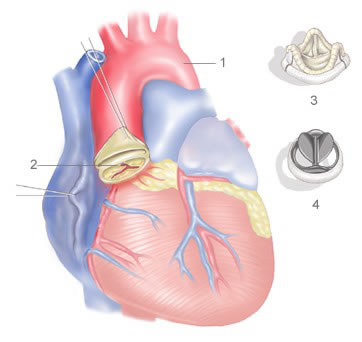
Biological valves are less durable, especially in the young, but they carry a lower risk of developing clotting problems, and therefore do not require lifelong use of anticoagulant medicine (warfarin).
Patients with a stenotic aortic valve will need to have valve replacement surgery, as will patients with a regurgitant valve that is unsuitable for repair, as untreated both can lead to congestive heart failure.
Possible reasons for an aortic valve to become stenotic or regurgitant are age-related calcific deposits, degenerative valve disease, bacterial endocarditis and rheumatic fever. Lifestyle choices such as smoking and a high cholesterol diet can increase the risk of a stenotic aortic valve. Other risk factors include old age and diabetes.
Minimally-invasive (or key-hole) aortic valve replacement may be necessary for those whom more major surgery is unsuitable, possibly due to age, medical history and poor mobility. Minimally-invasive surgery is preferable in terms of recovery time, cosmetic results, reduced hospital stay, and results in fewer post-operative complications than conventional aortic valve replacement.
Aortic valve regurgitation and stenosis develop gradually, and your heart often compensates for the problems. You may have no signs or symptoms for years, and you may even be unaware that you have either condition.
The primary symptoms of both aortic valve regurgitation and aortic valve stenosis are: fatigue and weakness (esp. during physical activity), shortness of breath, chest pain, swollen ankles, heart palpitations and dizziness.
There are a number of ways to diagnose a regurgitant or stenotic aortic valve, including: an echocardiogram, exercise tests, an MRI scan of the heart, an electrocardiogram (ECG), and chest X-rays. If these non-invasive methods are inconclusive, you may also require cardiac catheterisation, in which a small catheter is threaded through blood vessels to the aorta and dye is injected in order to provide a very clear X-ray picture.
There is a recently pioneered non-surgical technique known as percutaneous or transcatheter aortic replacement (P/TAVR), that may be suitable for those unable to undergo surgery.
The recovery time for minimally-invasive aortic valve replacement is faster than that of conventional aortic valve replacement, usually 3-4 weeks, and results in less discomfort for the patient and a more stable breast-bone.
Outcomes for this surgery are as good as the more invasive aortic valve replacement, and it is a safe and well understood variety of cardiac surgery. There are less restrictions on heavy lifting after the operation compared to conventional surgery, and the operation results in a shorter hospital stay of around 4 days.
The survival rate after 30 days is around 98%, with only minor risks of complications. Over 90% of patients show excellent results, with either trace or no regurgitation post-operation.
Depending on which kind of valve prosthesis was used, patients may or may not be using anticoagulant medicine (warfarin) for life.

